Gender Critical activists are doing the opposite of good trauma advocacy
As someone who’s done my share of patient advocacy I’m pissed off

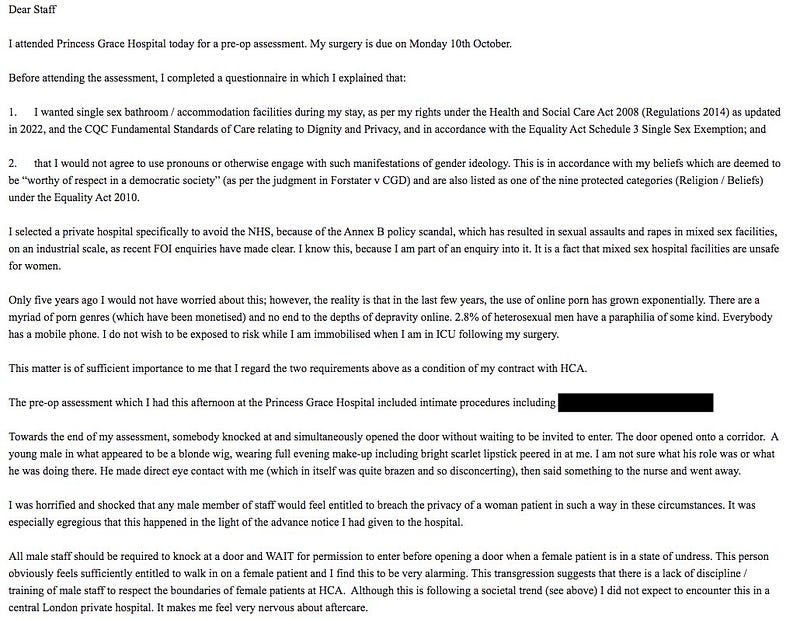
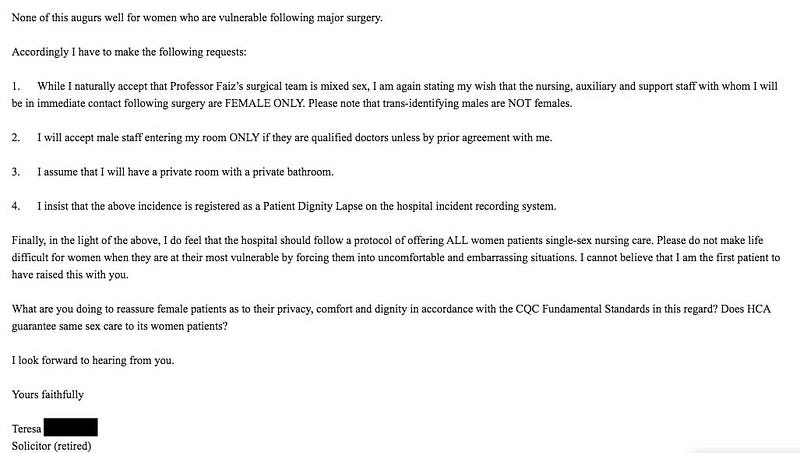
There’s a currently trending media story about a retired solicitor in need of surgical interventions who’s appointment date was cancelled because of a screed she submitted to the hospital which doesn’t actually mention her experiences of sexual violence at any point. It does however extensively discuss her opposition to “Gender Ideology” and to “using pronouns” and in it she claims, in a way I suspect does not hold legal water, a series of protected rights to demand service according to her “advance directive”.
I’ll post the email at the end, as published by her ally, Gender Critical researcher “@ripx4nutmeg”.
Takes on this particular case have predictably been polarised for and against the woman in question. Gender Critical figures are of course shocked that her appointment was cancelled and feel (in line with their beliefs that the protected status of “Gender Critical beliefs” in law enables virtually any level of demand made on this basis) that the hospital was completely out of order. Many health care professionals and trans allies have countered that the woman in question is obviously unreasonable, the resources aren’t there, that she is a “Karen”, that it’s not staff’s problem if she’s a bigot and so on. I’m a bit fraught personally.
I agree with those who would say that she’s being unreasonable — she makes it clear in the letter that she intends in advance to misgender or otherwise disrespect staff she believes might be trans (something no employer is legally allowed to knowingly subject their staff to, whether they are trans or not). She demands an “all-female” team of nursing and auxilliary staff while clearly stating “trans identifying males are not females” suggesting substantial headaches for management in terms of being being lawfully unable to ask their staff to disclose trans status and therefore unable to provide services that comply with her request, which she also makes clear she considers a form of contract on which her consent to healthcare is based.
In fact she goes further than that and demands a number of facilities like private room and private bathroom which the hospital make clear are simply not available in the intensive care ward on offer, the way that the hospital is built, and says that the hospital should offer this service to “all women patients”. All of this within the context of a rant that starts off quoting the high rates (she claims) of transvestic fetishism and pornography driven perversion among “males” and describes one of the staff she saw as “a young male in what appeared to be a blonde wig, wearing evening make-up including scarlet lipstick” — an obviously quite objectifying description of anyone — who she describes as “brazen” for having made eye contact with her. She does report quite reasonably a concern that this staff member knocked but failed to wait before entering during an investigation where she would have been exposed at one point. These things happen, but it’s a reasonable thing to complain about and ask to be addressed.
So what’s the problem? What is this about advocacy?
My problem with just saying “she’s being unreasonable” and leaving it there is that I’ve spent a lot of my life helping people who are in various states of being “unreasonable”. Friends, lovers, etc who have experienced trauma, particularly those who struggle to access healthcare for a wide range of reasons including discrimination and more importantly a history of discrimination leading to them experiencing an antagonistic relationship with healthcare professionals, have frequently needed support with attending appointments. I’ve spent a lot of time over my life sitting with someone else in doctors offices, talking to social workers or just sitting in on benefits assessments, with people who struggle to get what they need out of those services.
Trauma, a lifetime of experiencing discrimination and violence affect different people differently, but often none of the ways they affect people are good. We develop maladaptive coping strategies. Some people become more hostile, come to the conclusion that their health professionals are plotting against them. Others, particularly autistic people, can become non-verbal, physically unable to speak due to stress and fear brought up by experiences of trauma. Personally I tend to just avoid healthcare and meetings with doctors altogether, try to people please, and occasionally lose my shit in the middle of a medical exam in floods of tears because I failed to tell people what my personal damage is.
I do peer advocacy a lot less these days than I used to because I have less free time, but by way of explanation, the way it tends to work is that you have one person who needs help navigating a system that is traumatic for them, and you have another individual who because it is not your problem personally as an advocate, it is fundamentally less stressful for you, and you take on board the job of trying to translate the needs, and wishes of the person in need of care into a plan, potentially a short guide for professionals so that they understand what the individual is struggling with and how you plan to navigate around their trauma in the context of what services the health service in question is able to provide.
I won’t go into too many details about what sorts of adjustments people may need or be provided with. This can range over a whole variety of things like:
- Meeting professionals who will be involved long in advance so as to get used to the prospect of being vulnerable to them in a neutral environment,
- Set out clear boundaries on not receiving care from specific individuals the care receiver does not feel safe with, potentially,
- Making a clear written care plan so as to improve confidence in understanding what’s going to happen and iron out potential pain points,
- Have a trusted friend or family member help with aspects of a procedure which may be triggering when undertaken by a stranger (where safe to do so),
- Medical help with sedation in order to reduce the impact of specifically traumatic investigations when triggers are unavoidable.
None of this is medical advice, triggers are very personal, there can be a huge range of things which set people off or make things less challenging to undergo.
The core goal of peer advocacy and the hallmark of a GOOD peer advocate is to sift out the difference between anxiety, conspiracy theories that the person you’re advocating for is talking about, negative emotions tied up in facing the prospect of traumatic experiences surfaced from receiving healthcare, to separate those out from articulating what it is they actually say they require. You’re there to listen to them and help articulate what they are telling you they need while not repeating things that drag their care off the rails. In Teresa’s case that could include separating out rants about gender ideology, or pornography, that are not obviously to do with securing the individual’s healthcare needs, so much as they express fears and concerns that she has, from her request for female care staff or to ensure that knocking happens. It may also include getting in touch with the hospital and saying “okay, I understand that you can’t guarantee none of your staff are secretly trans, which is a worry of Teresa’s, but can you tell her who her team will be so that she can make the decision to go ahead with treatment or go elsewhere?” Fundamentally it’s about identifying what the stumbling blocks are for the person you are doing advocacy for, and finding a way, if possible, to communicate that and make that work with healthcare staff, while minimising friction for everyone.
Obviously not all “requirements” are feasibly possible, and sometimes the healthcare people need is not available, but the job of doing good advocacy is about being the person who is not so deeply triggered that you can listen to their needs and help articulate them honestly to a service provider in a way that doesn’t confuse the service provider into rejecting them.
Being traumatised makes people behave in confusing ways. Being triggered absolutely SUCKS. People in those states say and do things which are self-sabotaging and drag them off of what they had intended because they are set off with a reflex reacting to flashbacks or confrontational relationships and experiences that likely are not even happening in the present. Triggered people can become incoherent, inarticulate, disoriented, paranoid, combative, and even hallucinate! The nature of it is that people become less reasonable and less able to advocate effectively on their own behalf and that’s what I find so deeply upsetting about this story and the way it has polarised people.
It’s possible that “Teresa”, the woman who wrote the letter, is unwilling to get the healthcare she needs because of her ideological commitments. But if she’s acting out of trauma and without the support of an advocate of some kind who doesn’t have another political agenda (like her GC friends clearly do) she won’t find out if it’s possible to secure what it is she needs, and that’s extremely sad to me.
A lot of people have responded to this story by hoping she comes to harm because of the ways her choices and self-advocacy have obstructed her access to healthcare. I really strongly feel that even people who have done harm deserve access to care, and that it’s important that as a society we try and extend care to each other as far as possible. Everyone has a right to make bad decisions for the sake of their own health, and people wrestling with trauma are still responsible for their actions when that leads to them lashing out at others. Nevertheless, I think it’s important that we try to find ways to help people get what they need to heal and thrive, not address harmful attitudes and behaviours through retribution.
[Incidentally, if you’re interested in learning advocacy in a transfeminist and mad liberation framework, I highly recommend QueerCare’s training when it’s available as one of the few offerings I’m aware of in this space]